Five questions for … Dr. Huong Nguyen
A nurse and health services researcher, Huong Q. Nguyen, PhD, RN, focuses her research on the care of older adults with chronic and serious illnesses. She is the co-lead of the Care Improvement Research Team and interim director of the Division of Health Services Research & Implementation for the Department of Research & Evaluation. She is also a professor in the Department of Health Systems Science of the Kaiser Permanente Bernard J. Tyson School of Medicine.
You are unique in our research department as a nurse who became a full-time research scientist. Tell us what led to you becoming a nurse, and then to becoming a research scientist?
I often joke about being an imposter nurse with my nursing colleagues, mostly because I provided direct patient care for less than a year! The backstory is that like many Asian parents, my parents also wanted my brother and me to pursue professions such as medicine. I wanted to appease my parents but knew that the economics of attending medical school didn’t really align with the limited resources of a struggling refugee family. I took the practical route of pursuing nursing as a profession to fall back onto if medicine did not work out. What shifted my views about nursing was my sophomore year summer research internship at the University of Wisconsin, Madison. I was most fortunate to work with a nurse scientist who ran her own wet lab to examine the biological mechanisms underlying cancer cachexia, (which is a wasting syndrome characterized by weight loss, anorexia, asthenia, and anemia) and intervening through nutritional support. Dr. Donna McCarthy was quite the pioneer and likely one of only a few PhD-prepared nurses in the mid-1990s who conducted translational research. That experience shifted my career aspirations entirely and I was fully committed to pursue graduate training in nursing research, knowing that I could improve the lives of more people in a completely different way. There are so many ways nurses, at all levels of training, contribute to the health of individuals and communities. Over the years, I have tried to blend the multiple disciplinary traditions of holistic patient care from nursing to systems thinking around population management to conduct impactful research for Kaiser Permanente Southern California members that also have implications outside of our organization.
You currently serve in two roles, interim director of Health Services Research and Implementation Science and co-lead of the Care Improvement Research Team. What are the biggest challenges and rewards?
Much of what I relish in my leadership role is connecting the dots on what’s important or pain points related to care delivery for the organization with the expertise and interests of our scientists and clinicians and brainstorming on how to collaboratively solve those challenges. The most rewarding scenarios are when we can use internal Kaiser Permanente Southern California funding to quickly answer a care delivery question for our leaders and at the same time secure more substantive external funding to further expand the research to generate generalizable knowledge and build up our reputation in a particular space. With our large, complex, matrixed governance structure, it can be challenging at times to align priorities and resources to mount regionwide research initiatives that could provide us more definitive answers to a particular care delivery question that is unique to KPSC and where external funding is not suitable. We do try to be creative and leverage the inherent variation that exists to understand practices that are associated with better outcomes.
You’ve been working with Nancy Gin, MD, on a PCORI initiative. Tell us about that project and what you hope to learn.
Dr. Gin is the Kaiser Permanente Southern California project lead in the Patient-Centered Outcomes Research Institute’s Health Systems Implementation Initiative (PCORI HSII), which was established in 2023 to reduce the lag between publication of research results shown to improve patient outcomes and their implementation in routine health care practice. Building on the exceptional foundation of evidence-based medicine practice in Kaiser Permanente Southern California, our organization will be able to compete for funding that could help facilitate implementation of new evidence-based practices that are aligned with organizational priorities over the next 5 years. As part of our capacity-building activities, we have developed a prioritization framework to help guide Dr. Gin, the Steering Committee, and our clinical-operational partners on which topics to pursue. We are also actively working on a playbook to support research and operational teams in submitting competitive funding proposals and if awarded, implement, and evaluate these new practices.
What research you are most proud of?
I was drawn to Kaiser Permanente more than 10 years ago for the grand opportunity to develop and test novel approaches to improve care for older adults with chronic and serious illness in real-world community settings. But little did I know how complex health care was then and even more so today. Nonetheless, much of my partnered research today remains aligned with those lofty goals and is further motivated by a selfish interest to ensure that by the time I need care, whether it’s in the outpatient, inpatient, and home care settings, I will receive high-quality, seamless, whole-person care that is aligned with my priorities.
Although we are continuing to chip away at this through different projects, the project I’m most proud of is our current pragmatic trial that tests a potentially scalable and sustainable practice support bundle to improve the detection of cognitive impairment and dementia in primary care. The project requires extensive engagement and partnership with multiple service line leaders and reflects the culmination of many lessons learned I’ve learned over the past 10 years in conducting embedded health systems research. I’m incredibly grateful to our very hard-working and dedicated research teams, clinical collaborators, and health system leaders and partners across my studies, who make all of this work possible.
What do you enjoy doing in your spare time when you are not at work?
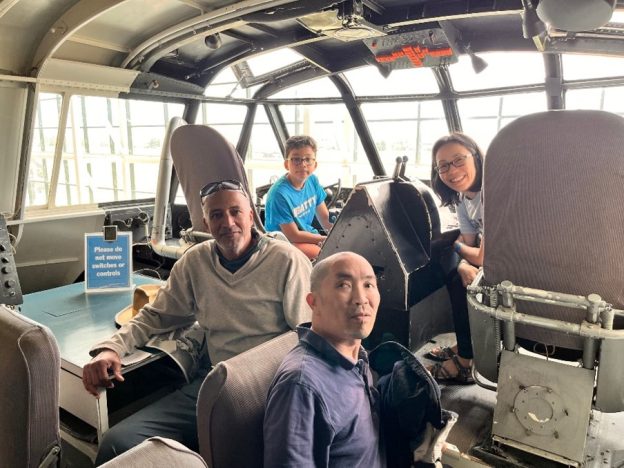
I enjoy every minute I get to hang out with my 13-year-old son, whether it’s trying to experience his coding programs in Roblox or Minecraft, watching him create public service announcement videos for his school, watching him practice how to do stalls in a glider plane, playing board games, cooking and exercising together—the weekends are never long enough!
Image: Dr. Huong Nguyen, her son Sydney, husband Tracy, and brother Phu in the Spruce Goose during their road trip up to the Pacific Northwest in summer of 2023.





