 Researchers tap into robust data systems to transform care
Researchers tap into robust data systems to transform care
FDA/Kaiser Permanente study highlights safety issues with arthritis drug
In 2001, David Graham, MD, MPH, from the Food and Drug Administration approached Kaiser Permanente about conducting a study that looked at safety of Vioxx, a COX-2 inhibitor used to manage pain and inflammation for conditions like arthritis.
The first COX-2 inhibitors were approved by the FDA in 1998 and 1999. They held appeal because they caused fewer gastrointestinal problems than other NSAIDs (nonsteroidal anti-inflammatory drugs). But in a pivotal trial by the manufacturer of Vioxx, concerns were raised about a possible link between Vioxx and heart attacks.
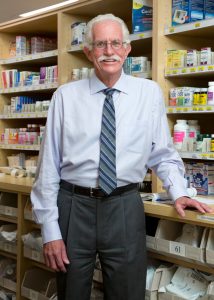 “Kaiser Permanente had taken a cautious approach to these drugs,” said Craig Cheetham, PharmD, who was tapped as the lead investigator for KPSC. “We and the SCPMG rheumatologists were already interested in looking at the potential health risks of Vioxx when the FDA approached us.”
“Kaiser Permanente had taken a cautious approach to these drugs,” said Craig Cheetham, PharmD, who was tapped as the lead investigator for KPSC. “We and the SCPMG rheumatologists were already interested in looking at the potential health risks of Vioxx when the FDA approached us.”
The researchers undertook a drug safety study, tapping into records for 1.4 million Kaiser Permanente members in Northern and Southern California who took anti-inflammatory medications, including ibuprofen, naproxen, Celebrex (a competing COX-2 inhibitor), and Vioxx. This study pre-dated the rollout of Kaiser Permanente HealthConnect® by several years, so the researchers primarily relied on a large data system called POINT.
“POINT wasn’t an electronic medical record, but it drew from about 400 different Kaiser Permanente computer systems to collect all available data on our patients,” said Dr. Cheetham, who worked in the Pharmacy Analytics Services Department at the time. “Back then, there weren’t a lot of health systems across the country that had linked these types of data that were used in the study.”
Preliminary findings drew significant attention from the media
In August 2004, the preliminary findings from the study were presented at a conference in France. The abstract and poster attracted an unusual amount of attention from the media.
The lead FDA scientist, Dr. Graham, told a congressional panel in November 2004 that the study found “that Vioxx increased the risk of heart attack and sudden death by 3.7-fold for high does and 1.5-fold for low dose compared to Celebrex.” With the widespread use of Vioxx he also emphasized that the death toll was equivalent to plane crashes at the rate of “2–4 aircraft every week, week in and week out, for the past 5 years.”
By the time Dr. Graham gave that testimony, the drug manufacturer had already withdrawn Vioxx from the market. The attention the FDA/Kaiser Permanente study received led the drug manufacturer to conduct an interim analysis on an ongoing clinical trial which also found elevated risk of heart attacks with the high dose.
The study was published in The Lancet in January 2005.
“It is unusual for a drug to be pulled from the market so quickly,” said Dr. Cheetham. “Our paper was published months later and after FDA and Congressional hearings.”
One of the benefits of the experience was that it helped raise awareness of the contributions the Kaiser Permanente pharmacy researchers could make to Kaiser Permanente research.
“I got more involved with R&E and also the Division of Research up in Northern California,” he said. “The Vioxx experience opened a lot of doors.”
Total Joint Registry aimed for quality improvement
 In 2001, KPSC research took another leap forward with the founding of the Total Joint Registry in San Diego. Clinical quality registries are intended to enhance quality, safety, and cost reduction using real-world data for a self-improving health system.
In 2001, KPSC research took another leap forward with the founding of the Total Joint Registry in San Diego. Clinical quality registries are intended to enhance quality, safety, and cost reduction using real-world data for a self-improving health system.
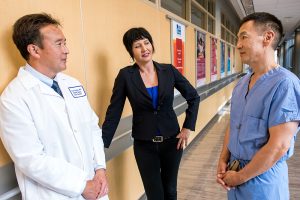
“We developed the Total Joint Registry in response to changing our national contracts for implants,” recalls Liz Paxton, PhD, MA, senior director of the data reporting, analytics, medical device surveillance, assessment unit of Clinical Analysis. “The physicians were concerned that if they switched implants, there could be some potential harm to patients.”
She said they saw the Total Joint Registry as an opportunity to develop a quality improvement mechanism in joint replacement where they could identify patient characteristics, surgical techniques, and outcomes primarily focused on revision, surgery, infections, complications, readmissions, emergency department visits, and deaths.
“We modeled the Total Joint Registry as a pilot study in San Diego after the Swedish hip registry,” Dr. Paxton said. “The Swedish registry had found they were able to change and improve outcomes on a national basis by providing feedback to physicians. We wanted to replicate that.”
Early successes led to expansion. In 2002 the program extended to all Southern California, and other regions were brought on the next year. The registry expanded to ACL, spine, shoulder, hip fracture, then cardiac and vascular devices and other specialties and implants.
Registry supports robust research, improved patient safety
Their first study, “Obesity and Perioperative Morbidity in Total Hip and Total Knee Arthroplasty Patients,” was published in 2005 in the Journal of Arthroplasty, identifying risk factors for revision surgery.
The registry has had a significant impact on patient safety by identifying orthopedic clinical best practices and disseminating this information to enhance quality of care. The registry model was adapted to other medical devices as well.
“For example, in 2015 there was a vascular device that our physicians were concerned about, and we evaluated it and found a higher-than-expected adverse event rate, Dr. Paxton said. “We notified the FDA, and our physicians agreed the internal evidence was strong enough that they stopped using it in 2016.”
Later that same year, the FDA distributed the first safety advisory on the device. The team’s research was published in the Journal of Vascular Surgery in 2021 and 2022.
Dr. Paxton said the implant registries ’success can be attributed to the overwhelming 95% participation by physicians, the support of regional and interregional chiefs’ groups, and the fact that patients stay with Kaiser Permanente for many years. Over 20 years, they’ve lost only 8% of membership in their registries.
Now, they are tracking about 4 million devices for over 800,000 patients. By 2024, they had published 290 articles in peer-reviewed journals.
A recently published paper that looked at the first 20 years of the implant registries concluded, “The use of implant registries within our health system, along with clinical leadership and organizational commitment to a learning health system, was associated with improved quality and safety outcomes and reduced costs.”
R&E focuses on expanding scientific ranks
 Meanwhile, the R&E focused on recruiting scientists. In 1999, there were 7 investigators in R&E. By 2002, that number had increased to 11. One of those recruits was Reina Haque, PhD, MPH, who came to R&E from UC Berkeley.
Meanwhile, the R&E focused on recruiting scientists. In 1999, there were 7 investigators in R&E. By 2002, that number had increased to 11. One of those recruits was Reina Haque, PhD, MPH, who came to R&E from UC Berkeley.
Dr. Haque’s focus at UC Berkeley was on international research projects. However, Kaiser Permanente was in her blood. Her great uncle had worked for Henry J. Kaiser as an engineer, and she had been a Kaiser Permanente member since birth. Also, she had family in Pasadena and thought it would be a good place to raise her own.
“The big draw, though, was establishing an independent career,” Dr. Haque said, “Having support, but working on projects I wanted to work on. Leadership truly wanted to know our opinions about certain clinical dilemmas and programs. We had access to leadership and often talked about how our projects could help clinical practice. We also had opportunities to partner with clinicians.”
She said that at the time, Dr. Petitti’s vision was for the scientists to be a small group with specialized research areas: cancer, clinical epidemiology, diabetes, behavioral outcomes, women’s health and reproductive health, and health services research.
“We have become so much broader in terms of research subject matter and expertise,” Dr. Haque said. “Also, over time, the things we used to have to do on our own as scientists, like grant applications, we now have teams of people here to help us.”
Researchers join groundbreaking national projects

 Despite having a small staff in the early 2000s, the department joined in on several influential multicenter projects. One of those was SEARCH for Diabetes in Youth, a national study aimed at understanding more about diabetes among children and young adults. Dr. Haque said that study “helped put R&E on the map.”
Despite having a small staff in the early 2000s, the department joined in on several influential multicenter projects. One of those was SEARCH for Diabetes in Youth, a national study aimed at understanding more about diabetes among children and young adults. Dr. Haque said that study “helped put R&E on the map.”
Another influential multicenter project, the Hyperglycemia and Adverse Pregnancy Outcomes study, began enrolling in 2000. This one focused on gestational diabetes.
“When the HAPO study came along, I was the clinician on the project and part of the organizing committee,” Dr. David Sacks said. “We met in Chicago and hammered out details. Kaiser Permanente in Bellflower was one of the 5 centers in North America.”
The ongoing study eventually found a strong association between maternal glycemia and infant and childhood obesity being associated with type 2 diabetes and cardiovascular disease in adult life. The third phase of the study, HAPO for Cardiovascular Health, began recruiting in 2023.
HIV/AIDS clinical trials program provides critical access for patients
Although KPSC’s participation dates back to the 1980s, the formal program called the HIV/AIDS Research Trials program wasn’t established until almost 2 decades later. William Towner, MD, FACP, FIDSA, and Hai Linh Kerrigan, PharmD, founded the program in 2004.
“This program allows Kaiser Permanente to be on the cutting edge of scientific developments in HIV,” said Dr. Towner in an interview with the Kaiser Permanente HIV Health Matters newsletter in 2007. Dr. Towner is now the physician director of the Division of Clinical Trials Research.
At the time, access to investigational drugs was vital to people living with HIV/AIDS, particularly if they were no longer responding to other treatments that were available at the time.
“We don’t conduct clinical trials just for the sake of research; we do them as part of our standard of care. We owe this access to our patients,” Dr. Kerrigan said in the same edition of HIV Health Matters. Dr. Kerrigan is now the division research administrator for clinical trials.
Since the start of the AIDS epidemic, KPSC has served as a research site for nearly 100 HIV clinical trials, enrolling hundreds of patients and taking part in the development of every compound currently available to treat HIV.
The HART program later evolved into a broader program focused on infectious diseases, helping to advance treatment and prevention of many other diseases, including hepatitis, Clostridioides difficile, influenza, and more.
An era of exponential growth for research
 In 2004, Michael Kanter, MD, who had been doing research as a clinician since the mid-1980s, became regional medical director of Quality and Clinical Analysis for SCPMG. Part of that job was overseeing R&E with support from others.
In 2004, Michael Kanter, MD, who had been doing research as a clinician since the mid-1980s, became regional medical director of Quality and Clinical Analysis for SCPMG. Part of that job was overseeing R&E with support from others.
“Our research has truly been a benefit for patients,” Dr. Kanter said. “As a learning health care organization, we generate learning from the care we gave to patients. That’s why R&E works so well. There’s a certain number of doctors who join Kaiser Permanente because they want to do research. We would lose a lot of talented physicians if they didn’t have that opportunity.”
When Dr. Petitti left the department, a search began for a new leader. Dr. Kanter wanted someone who could grow the department, lead research that was relevant to clinical care at Kaiser Permanente, and bring in funding to support the growing body of research. In 2005, he interviewed Steven Jacobsen, MD, PhD, who was then leading the epidemiology department at Mayo Clinic.
Integration of research and clinical practice
Dr. Kanter said Dr. Jacobsen’s work was to expand the department without a large budget, which meant bringing in funding to support the growing body of research. Dr. Jacobsen recalls with excitement the opportunities and challenges of leading what was then a “really small research shop without a lot of infrastructure.”
 “Dr. Kanter’s directive was he wanted it to grow, but also to grow so it was more integrated into practice,” Dr. Jacobsen said. “With each scientist I hired, I was looking for fire in the belly. I looked for passion for the possibility of leveraging our data and the health care system to answer important questions that could lead to changes in health.”
“Dr. Kanter’s directive was he wanted it to grow, but also to grow so it was more integrated into practice,” Dr. Jacobsen said. “With each scientist I hired, I was looking for fire in the belly. I looked for passion for the possibility of leveraging our data and the health care system to answer important questions that could lead to changes in health.”
Kristi Reynolds, PhD, MPH, who Dr. Jacobsen hired as a research scientist, remembers the enthusiasm and exhilaration of that time. “I was excited to join R&E because of Steve’s mandate to grow the department and all the possibilities to come,” said Dr. Reynolds, who is now the director of Epidemiologic Research. “I saw a lot of opportunities to collaborate internally. I was very excited about the chance to work in a learning health care system and potentially see my research findings implemented to address knowledge gaps and ultimately lead to better health outcomes.”
Dr. Jacobsen sought to expand cardiovascular research and to bring in-house the vaccine research being done in collaboration with the Vaccine Safety Datalink. Around 2008, Dr. Jacobsen became a principal site investigator for the Vaccine Safety Datalink, which was making important discoveries then and became even more high profile over a decade later during the COVID-19 pandemic.





